ADVERTISEMENT
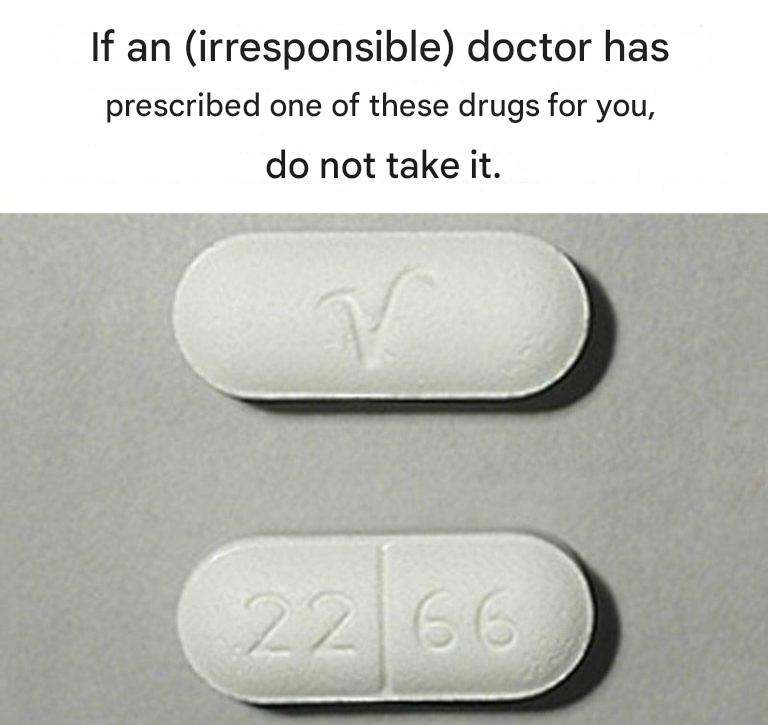
If a Doctor Ever Prescribed You One of These Medications, You Should Read This Immediately
Most of us trust prescriptions without a second thought. A doctor writes a name on a pad or clicks a few buttons, the pharmacy hands over a small bottle, and we assume that what’s inside is both necessary and safe—because why wouldn’t it be?
But here’s the uncomfortable truth: some of the most commonly prescribed medications in the world come with risks that many patients are never fully told about. Not because doctors are malicious or careless—but because modern medicine is complex, rushed, and often built around symptom management rather than long-term outcomes.
This article is not meant to scare you or convince you to stop taking medication. Instead, it’s meant to inform you, empower you, and encourage smarter conversations with your healthcare providers.
If you’ve ever been prescribed any of the medications discussed below—or medications in these categories—you should read this carefully.
Why This Matters More Than Ever
Prescription drugs save lives every day. Antibiotics, insulin, blood-pressure medications, and countless others have transformed modern healthcare. However, no medication is risk-free, and some are prescribed so frequently that their dangers are underestimated or overlooked.
Three major issues contribute to this problem:
Time-limited doctor visits – There’s often little room for in-depth explanations.
Outdated assumptions – Some drugs were approved decades ago, before long-term risks were fully understood.
Normalization of side effects – Many adverse effects are dismissed as “just part of treatment.”
Understanding what you’re taking—and why—can be just as important as taking it correctly.
Important Disclaimer
This article is not medical advice.
You should never stop, start, or change a medication without consulting a qualified healthcare professional.
The goal here is education—so you can ask better questions and make informed decisions.
- Benzodiazepines (Anxiety & Sleep Medications)
Common examples:
Xanax (alprazolam)
Valium (diazepam)
Ativan (lorazepam)
Klonopin (clonazepam)
Why They’re Prescribed
Benzodiazepines are often prescribed for:
Anxiety
Panic attacks
Insomnia
Muscle spasms
Seizures
They work quickly and effectively—sometimes too effectively.
What Many Patients Aren’t Told
Benzodiazepines can cause:
Physical dependence (even at low doses)
Severe withdrawal symptoms
Memory impairment
Increased risk of falls (especially in older adults)
Cognitive decline with long-term use
Withdrawal can be dangerous and long-lasting, sometimes lasting months or even years.
What to Ask Your Doctor
Is this intended for short-term or long-term use?
What’s the exit plan?
Are there non-drug alternatives?
- Opioid Painkillers
Common examples:
Oxycodone
Hydrocodone
Morphine
Fentanyl (medical use)
Why They’re Prescribed
Opioids are powerful pain relievers used for:
Post-surgical pain
Chronic pain
Cancer-related pain
The Hidden Risks
High addiction potential
Rapid tolerance (needing higher doses)
Respiratory depression
Increased sensitivity to pain over time
Overdose risk—even when taken as prescribed
Many people who developed opioid dependence started with legitimate prescriptions.
Critical Questions
Is this the lowest effective dose?
How long should I take this?
Are there non-opioid pain management options?
- Proton Pump Inhibitors (PPIs) – Acid Reflux Drugs
Common examples:
Prilosec (omeprazole)
Nexium (esomeprazole)
Protonix (pantoprazole)
Why They’re Prescribed
PPIs reduce stomach acid and are prescribed for:
GERD
Acid reflux
Ulcers
What Long-Term Use May Do
Long-term PPI use has been associated with:
Nutrient deficiencies (magnesium, B12)
Increased fracture risk
Kidney disease
Increased infection risk
Rebound acid hypersecretion
Many people stay on PPIs for years when they were intended for short-term use.
Ask Your Doctor
How long should I be on this?
Can I taper off?
Are lifestyle changes an option?
- Antidepressants (SSRIs & SNRIs)
Common examples:
Prozac
Zoloft
Lexapro
Effexor
Why They’re Prescribed
Used for:
Depression
Anxiety
OCD
PTSD
Chronic pain
What Patients Often Discover Later
Emotional blunting
Sexual dysfunction
Weight changes
Withdrawal symptoms (“discontinuation syndrome”)
Difficulty stopping the medication
Not everyone experiences these—but many are not warned beforehand.
Important Questions
What side effects should I expect?
What happens if I want to stop?
Are therapy or lifestyle interventions part of the plan?
- Statins (Cholesterol-Lowering Drugs)
Common examples:
Lipitor
Crestor
Zocor
Why They’re Prescribed
Statins lower cholesterol and reduce cardiovascular risk.
Possible Side Effects
Muscle pain and weakness
Fatigue
Blood sugar changes
Memory issues (in some people)
For some patients, benefits clearly outweigh risks. For others—especially low-risk individuals—the decision may deserve deeper discussion.
Ask Your Doctor
What is my actual cardiovascular risk?
Are lifestyle changes enough?
What symptoms should I watch for?
- Hormonal Birth Control
Forms include:
Pills
Patches
Rings
Injections
Why It’s Prescribed
Pregnancy prevention
Hormonal regulation
Acne
Endometriosis
What’s Often Downplayed
Blood clot risk
Mood changes
Libido changes
Nutrient depletion
Masking underlying hormonal issues
Hormonal birth control can be helpful—but it’s not benign.
Ask Your Provider
What are the risks for my age and health?
Are non-hormonal options available?
What symptoms should prompt reevaluation?
- ADHD Stimulants
Common examples:
Adderall
Ritalin
Vyvanse
Why They’re Prescribed
To improve focus, impulse control, and attention.
Potential Issues
Appetite suppression
Sleep disruption
Cardiovascular strain
Dependency risk
Emotional flattening
These medications can be life-changing for some—and problematic for others.
Ask Your Doctor
What monitoring is required?
What happens if I stop?
Are behavioral strategies part of treatment?
Why Informed Patients Do Better
Studies consistently show that patients who:
Understand their medications
Ask questions
Monitor side effects
Participate in decisions
…have better outcomes.
This isn’t about distrust. It’s about partnership.
How to Protect Yourself (Without Panic)
Here’s what you can do—starting today:
- Read the Medication Guide
Not just the label. The full insert.
- Keep a Medication List
Include:
Dose
Start date
Purpose
Side effects
- Ask “What’s the Long-Term Plan?”
Every medication should have a review point.
- Report Side Effects Early
Don’t wait. Even “minor” ones matter.
- Get Second Opinions When Needed
For Complete Cooking STEPS Please Head On Over To Next Page Or Open button (>) and don’t forget to SHARE with your Facebook friends
ADVERTISEMENT